+919360391740
gastrosurgeondrkumar@gmail.com
Rectal Prolapse
- Home
- Rectal Prolapse
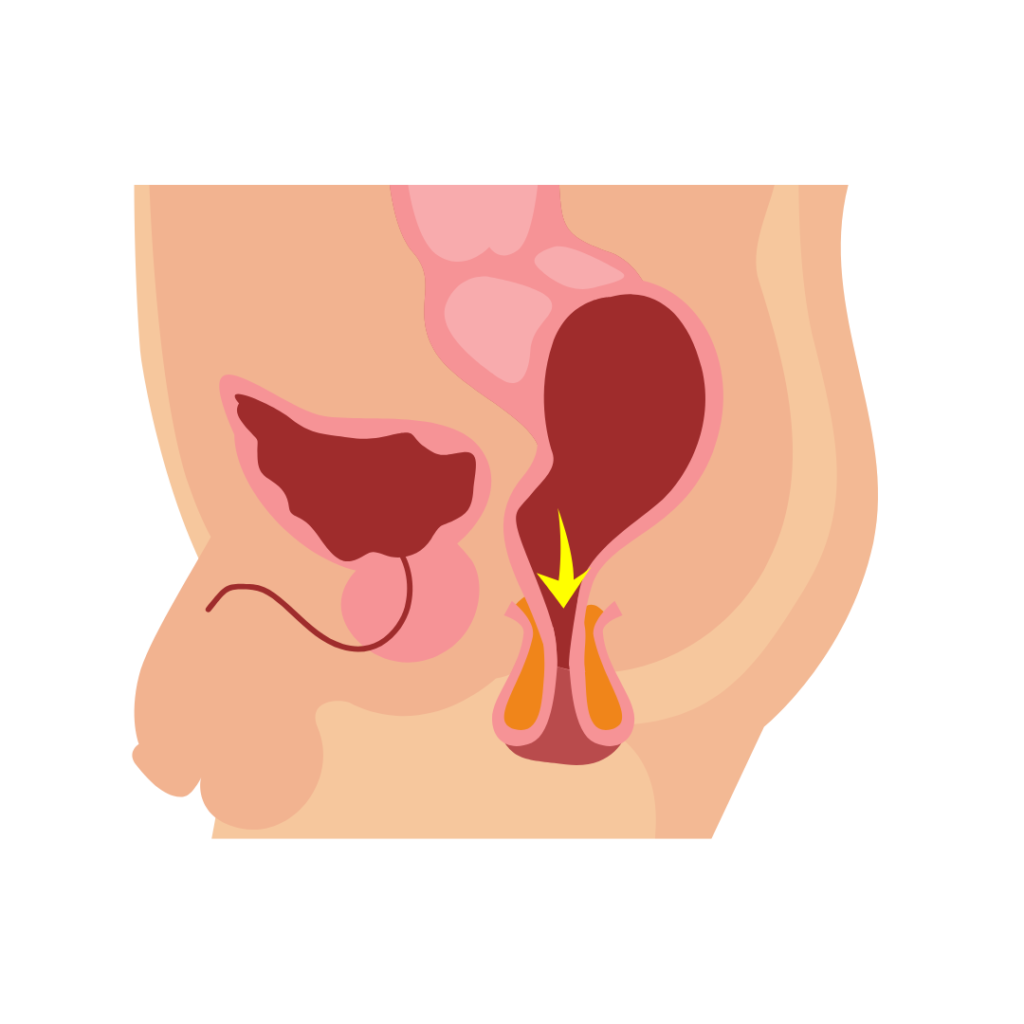
Any bodily part that slides or reclines from its natural position is said to prolapse. Rectal prolapse occurs when the rectum, the last segment of the large intestine, slips out of the anus.
Stages Of Rectal Prolapse
External Prolapse: The whole rectum protrudes from the outside of the anus.
Mucosal Prolapse: A portion of the rectal lining protrudes from anus in a mucosal prolapse.
Internal Prolapse: The rectum has begun to descend, but it is not yet protruding from the anus.
Signs And Symptoms
When straining during a bowel movement, patients may observe a bright red mass emerging from the anus.
The bulge can stay visible or it might slide back within the anus.
Additional signs and symptoms might be:
Faecal incontinence is the inability to regulate one’s bowel motions. loose stools or constipation. dripping mucus or blood from the stomach. having the sensation that the rectum isn’t emptied after passing gas.
Diagnosis
A quick clinical history of symptoms is taken, and then the rectum is examined. During the examination, the doctor might ask about coughing or strain.
Proctoscopy: A digital rectal examination is conducted, and then a proctoscopy (scope-inserted visualization of the rectum) is done.
MRI Defecography: The results of an MRI defecography test indicate the amount, quality, and efficiency with which the rectum can contain and expel faces.
Colonoscopy: Using a flexible tube with an integrated camera, this procedure examines the colon and large intestine. To rule out any related conditions, this is done.
Anal Manometry: The ability of the anal sphincters to shut tightly is measured by this test.
Surgical Management For Rectal Prolapse
There are many forms of rectal prolapse surgery that are performed to reposition the rectum. Your age, the severity of the ailment, and general health will all play a role in the type of surgery your doctor suggests. The two most typical surgical specialties are:
Abdominal Procedures
Open Rectopexy :An incision is made in the abdomen (belly) by the doctor during an abdominal rectopexy, which may involve bowel resection. The rectum is pulled into the sacrum, the rear wall of the pelvis, and stitched permanently, sometimes with a mesh sling to keep it in place. The rectum is held in place by the formation of scar tissue over time. Additionally, the doctor could operate on a colectomy (removal of part of the colon). By removing a portion of the large intestine, this treatment relieves persistent constipation.
Laparoscopic Rectopexy: The doctor makes 3 to 4 small abdominal incisions and inserts a thin tube with a laparoscope and medical equipment. After that, doctors fix the rectum in position. Another option is a bowel resection.
Perineal Procedures
The Altemeier operation involves the doctor pulling the prolapsed rectum through the anus and part of the sigmoid colon, which is the last segment of the large intestine connecting to the rectum. These parts are cut and removed during a proctocolectomy. The remaining portion of the rectum is then joined to the large intestine. In order to strengthen the muscles of the pelvic floor, they could also stitch them together more tightly (keratoplasty).
Delorme method: The surgeon removes the lining of the rectum for rectal mucosa prolapses or minor rectal prolapses. The rectum’s muscle layer is then folded over and stitched together inside the anal canal. The rectum is held in place by this doubled muscle wall.
DR.KUMARAGURUBARAN is one of the Best Doctor in treating patients with RECTAL PROLAPSE and has huge experience in LAPAROSCOPIC RECTAL PROLAPSE REPAIR.
Services
- Gerd - Gastroesophagel Reflux Disease
- Hiatus Hernia
- Endoscopy & Colonoscopy
- Cholelithiasis ( Gallbladder Stones)
- Appendicitis
- Jaundice
- Obesity
- Liver Cirrhosis
- Pancreatitis
- Inguinal Hernia
- Umbilical Hernia
- Ventral Hernia / Incisional Hernia
- Anal Fissure
- Anal Fistula / Fistula In ANO
- Hemorrhoids Or Piles
- Laparoscopic Surgery
- Rectal Prolapse
- Gist's - Gastrointestinal Stromal Tumors
- Inflammatory Bowel Disease - IBD -Ulcerative Colitis- Crohns's Disease
- Bowel Perforation - Intestinal Perforation
- Bowel Obstruction - Intestinal Obstruction
- Gastrointestinal Bleeding
- Liver Disorders
- Liver Cancer Hepatoma
- Gastric Disorders
- Stomach Cancer
- Small Bowel Disorders -Small Bowel Intestine Disorders Intra Abdominal Adhsesions
- Small Bowel Cancer ( Small Intestine Cancer)
- Large Intestine- Colon Disorders
- Colon Cancer
- Rectal Cancer
- Meckel's Diverticulum
- Spleen
